2023.01.02 | Questions 17-18
A toddler with multiple fractures
Hello,
I wanted to wish you all the best for 2023. A special thanks to everyone who worked in the hospital during this holiday season.
Feedback or comments are always welcome. My email is studyraregenetics@gmail.com.
Please feel free to forward this newsletter with anyone who might find it useful!
-Daniel
Questions
Question 17
A 18-month-old boy presents to the hospital with inconsolability and swelling of the right thigh after falling. He is just starting to learn how to walk. Initial radiographs reveal a fracture of the right femur and osteopenia. A follow-up skeletal survey is notable for fractures of the left lateral malleolus and right radius, as well as multiple Wormian bones in the lambdoid suture. Labs reveal normal serum alkaline phosphatase, calcium, phosphate, and vitamin D. His height is at the 1st percentile, while weight and head circumference are at the 40th percentile. Skin exam reveals a bruise on the right thigh with no other birthmarks or signs of trauma. His social and verbal development is as expected. Child protective services has a low suspicion for non-accidental trauma after a thorough evaluation. This patient is most likely affected with which of the following disorders?
Question 18
Genetic testing is sent and reveals a stop-gain (nonsense) variant in COL1A1, confirming the diagnosis of osteogenesis imperfecta. In addition to recurrent fractures, this infant is at risk for which of the following complications as an adult?
Explanation
The patient in Question 17 has osteogenesis imperfecta (OI), a skeletal disorder that predisposes to fractures with minimal or no trauma. The word “osteogenesis imperfecta” reflects the defective (i.e. imperfect) bone (‘osteo-’) formation (‘-genesis’) seen in this disorder. Fractures commonly occur in long bones, though can occur in any bone. On radiography, patients with OI may have multiple fractures, low bone mineral density, and Wormian bones in the cranial sutures (due to abnormal ossification). The age of presentation and severity of symptoms in OI is highly variable, ranging from multiple fractures in utero to 1-2 fractures in adulthood.
As patients with OI age, they are at risk for hearing loss (Question 18). This can be due to atrophy or fracture of the auditory ossicles (aka the middle ear bones), which are the 3 smallest bones in the body. In addition to recurrent fractures, patients may also have scoliosis, bowing of long bones, short stature (as in this patient), blue sclera, dentin defects 😬, and joint laxity / hypermobility. Patients with OI may have delayed gross motor milestones (e.g. walking late, as in this patient) and otherwise are expected to meet cognitive milestones.
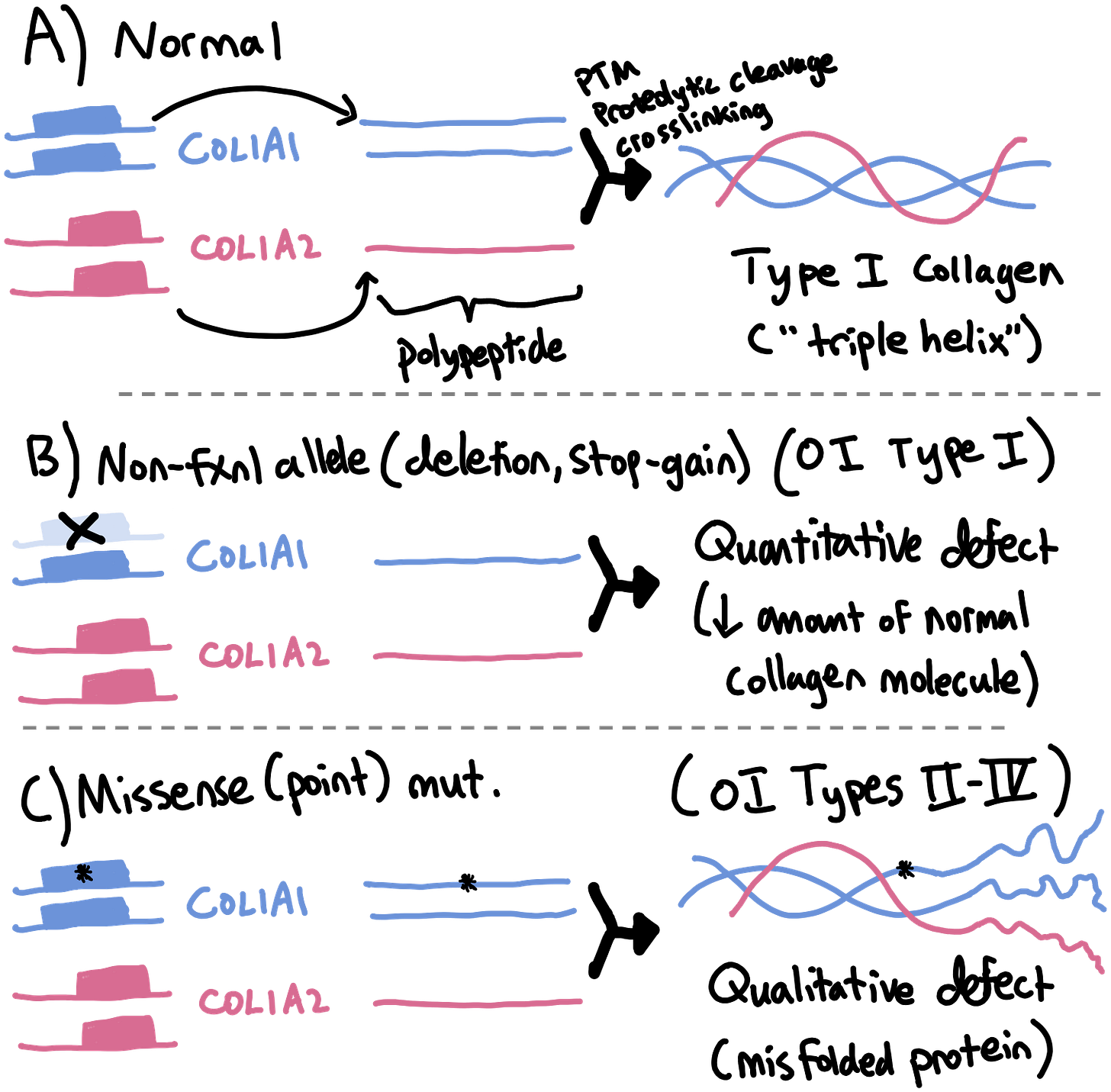
Collagen
Most cases of OI (~90%) are due to dominant mutations in the two genes (COL1A1 & COL1A2) that encode type I collagen, an extracellular protein that structurally supports bone and other connective tissue. Type I collagen is composed of 3 intertwined polypeptides that form a triple helix (see figure below). The other 10% of cases of OI are caused by (mostly) recessive mutations in one of nearly 20 genes involved in the function of osteoblasts (collagen-producing bone cells) or the post-translational modification, proteolytic cleavage, or crosslinking of collagen.
💡 There are 5 main types of collagen (I-V). Type one collagen is the most abundant protein in bone (hence the increased risk for fractures with type I collagen defects).
Patients with heterozygous deletions or stop-gain (nonsense) mutations in 1 copy of COL1A1 or COL1A2 produce ~50% less collagen, resulting in osteogenesis imperfecta type I. In contrast, heterozygous missense variants in COL1A1 or COL1A2 act in a dominant-negative manner, resulting in formation of an abnormal collagen that activates the unfolded protein response and damages osteoblasts. This leads to osteogenesis imperfecta types II-IV, which are more severe forms of OI that present in utero or in the neonatal period.
💡 The quote “It is better to be alone than to be in bad company” is as true for collagen as it is for our interpersonal relationships. COL1A1 alleles with missense variants are bad company!
Management
Treatment for OI is supportive and symptomatic. Bisphosphonates, approved for use in osteoporosis, are used off-label to improve bone mineral density, though a reduction in fractures has not been clearly demonstrated in OI. Patients need close orthopedic and dental surveillance and should avoid contact sports. Hearing loss is managed symptomatically. Though no specific treatment is available for OI, advances in gene and cell therapy may bring new treatments for OI in the future.
Incorrect answers
Achondroplasia is due to mutations in the fibroblast growth factor receptor 3 (FGFR3) gene. Achondroplasia is associated with rhizomelic short stature, bowing of the legs, and macrocephaly but is not associated with an increased risk for bony fracture.
Infantile hypophosphatasia presents before 6 months of age with skeletal fractures and bone hypomineralization. Patients may also have bowed legs, failure to thrive and delayed motor milestones. The defining marker of this disease is low alkaline phosphate levels, which are not seen in the patient in question 17.
McCune-Albright syndrome can cause fibrous dysplasia of bone, which can predispose to fractures. Patients with McCune-Albright also have cafe-au-lait macules and endocrine anomalies (e.g. early puberty), neither of which were mentioned in this question. On radiographs, fibrous dysplasia is characterized by one or more intramedullary, expansile lesions with well-defined borders rather than by hypomineralization.
Learning objective
Osteogenesis imperfecta (“brittle bone disease”) is a disorder of type I collagen with a wide spectrum of severity. Symptoms include recurrent fractures with minimal trauma, hearing loss, short stature, dentin defects, and scoliosis. A child with multiple or recurrent unexplained fractures may prompt investigation by both child abuse and clinical genetics teams.
2023 ABMGG General Exam Blueprint | V. Single Gene Inheritance → d. Single Gene Disorders → i). Connective tissue disorders and ii). Skeletal dysplasias.

