2023.02.25 | Questions 32-33
Cancer Genetics (1/3) - Colorectal cancer & microsatellite instability
Hello,
This is the first in a series of 3 posts related to cancer genetics. Please feel free to email with any comments or questions. My email is studyraregenetics@gmail.com.
Also, please share this post with any colleagues who might find it useful!
-Daniel
Questions
Question 32
A 42-year-old man presents with weight loss and dark-colored stools for the past 2 months. He undergoes colonoscopy, which reveals a tumor in the ascending colon. An analysis of the tumor reveals a high degree of microsatellite instability, and subsequent evaluation is consistent with metastatic colorectal cancer. Which class of therapeutics could be considered for this patient?
Question 33
Germline genetic testing is sent for the patient in Question 32 and reveals a heterozygous pathogenic mutation in MLH1. The patient’s clinical presentation and genetic test result is consistent with which of the following disorders?
Explanations
Answer to Q32: Immune checkpoint inhibitors
Answer to Q33: Lynch syndrome
This patient presents with invasive colorectal cancer with a high degree of microsatellite instability (MSI). Microsatellites are short (1-9 base pair), repeating DNA sequences found within noncoding regions throughout the genome that are prone to mutation during DNA replication. Normally, the DNA mismatch repair (MMR) system recognizes and repairs insertions, deletions, and mis-incorporation of bases that naturally arise during DNA replication. However, when MMR is defective, DNA replication errors cannot be effectively repaired. MSI is a marker of defective MMR and is associated with the accumulation of numerous mutations across the genome, not only within microsatellites. MSI is seen in ~20% of all patients with colorectal cancer, and is commonly seen in the tumors of patients with Lynch syndrome (Question 33), a disorder due to defective MMR. MSI can also occur sporadically in patients without Lynch syndrome.

Lynch syndrome results from defective MMR
Lynch syndrome, also known as hereditary non-polyposis colorectal cancer (HNPCC), is the most common cause of hereditary colorectal cancer. Lynch syndrome also increases the risk of developing multiple other types of cancer including endometrial, gastric, ovarian, and brain cancer. Lynch syndrome is inherited in an autosomal dominant manner and is caused by germline variants in genes that encode DNA MMR proteins. These genes include MLH1 & MSH2 (90% of cases), MSH6 (7%), and PMS2 (<5%). Deletions (not point mutations) of EPCAM can also cause Lynch syndrome.
Individuals with Lynch syndrome should undergo increased cancer screening, including earlier and more frequent colonoscopies and gynecologic exams, to detect and treat cancer at an early stage. Additionally, some patients with Lynch syndrome undergo prophylactic surgery to remove certain at-risk organs (e.g. uterus, ovaries) where there are no good cancer screening options available.
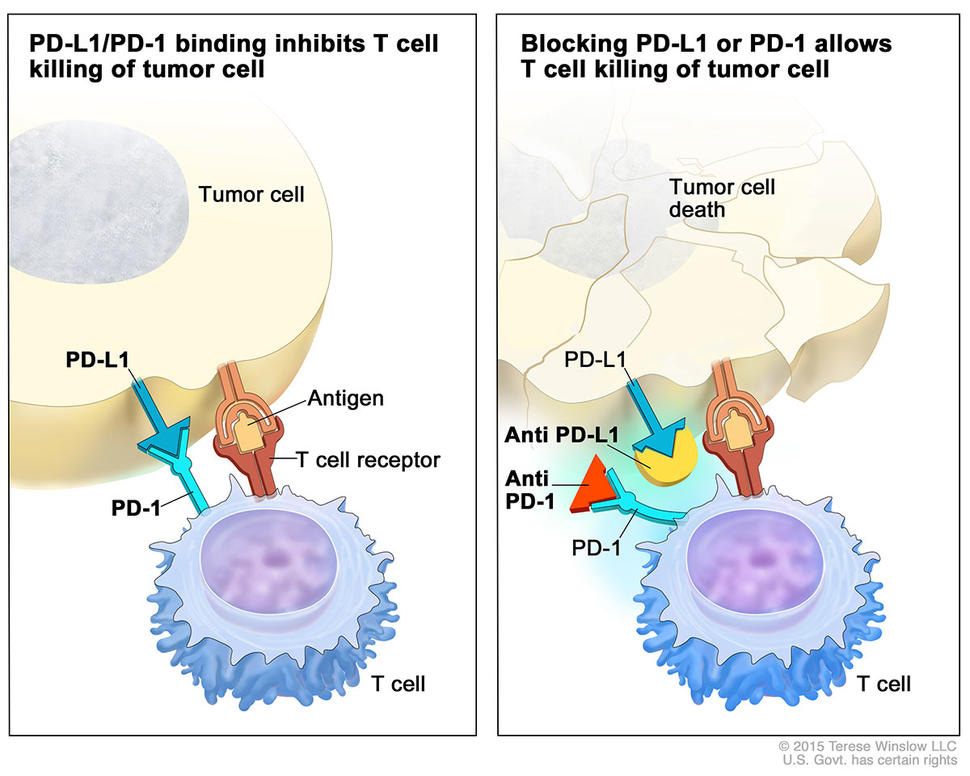
Immune checkpoint inhibitors (ICIs) treat tumors with MSI / MMR defects
Tumors with MSI and defective MMR (as seen in Lynch syndrome) are more likely to have an increased number of somatic mutations, which can lead to the production of abnormal proteins that are recognized by the immune system as foreign. Therefore, immune checkpoint inhibitors (ICIs), which activate the immune system to target and kill cancer cells, are effective in treating tumors with a high degree of microsatellite instability (MSI-H) resulting from defective MMR. ICIs work by blocking the interaction between the programmed death receptor-1 (PD-1) protein on T-cells and its ligand PD-L1 on cancer cells, thereby preventing cancer cells from evading immune surveillance (see image below). Examples of ICIs include pembrolizumab (Keytruda), an antibody that inhibits the PD-1 receptor on T-cells. Pembrolizumab is used as first-line treatment for patients with metastatic MSI-H or MMR-deficient colorectal cancer, and is also approved for a variety of other cancers.
Incorrect answers (Question 32)
mTOR inhibitors target the mammalian target of rapamycin (mTOR) pathway, which promotes cell growth and division. mTOR inhibitors such as everolimus are used for tumors associated with tuberous sclerosis but not for tumors with MSI. PARP inhibitors (e.g. olaparib, rucaparib) are used in patients with germline or somatic BRCA1/2 mutations who have breast, ovarian, and pancreatic cancers. (Note that PARP inhibitors contain the phrase ‘par,’ as in olaparib). Tamoxifen is an example of a hormone receptor modulator — more specifically, a selective estrogen receptor modulator (SERM) — that is used to treat hormone receptor-positive breast cancer but not colorectal cancer.
Incorrect answers (Question 33)
Li-Fraumeni syndrome (LFS) is caused by mutations in the TP53 gene, which encodes a tumor suppressor protein (think TP53 = “Tumor Prevention”). LFS increases the risk of developing several types of cancers, including breast cancer, brain tumors, leukemia, and sarcoma. Familial Adenomatous Polyposis (FAP) is caused by mutations in the APC gene (also a tumor suppressor) and predisposes to the formation of thousands of polyps in the colon and rectum that have a high likelihood of becoming cancerous. Individuals with FAP have an almost 100% chance of developing colorectal cancer by age 40; therefore, treatment is with prophylactic colectomy. Peutz-Jeghers syndrome is caused by mutations in STK11 and causes gastrointestinal polyposis with pigmented spots on the lips, buccal mucosa, and perianal region. Individuals with Peutz-Jeghers syndrome have an increased risk of developing several types of cancer, including colorectal, pancreatic, and breast cancer.
💡 In contrast to FAP, Lynch syndrome is not associated with a high number of polyps, hence the term hereditary “non-polyposis” colorectal cancer (HNPCC).
💡 Patients need A Prophylactic Colectomy (APC) if APC is mutated.
Learning objective
Lynch syndrome is the most common cause of hereditary colorectal cancer and is associated with a high degree of microsatellite instability in tumors. Immune checkpoint inhibitors (e.g. pembrolizumab) can be used to treat colorectal cancers with microsatellite instability due to their high mutation rates. Hereditary cancer predisposition syndromes such as Lynch typically arise from mutations in genes encoding tumor suppressor proteins and are most often inherited in an autosomal dominant manner.
2023 ABMGG General Exam Blueprint | VIII. Cancer genetics → b. Hereditary cancer predisposition → i. Autosomal dominant cancer predisposition syndromes (page 4)