2025.04.21 | Questions 94-95
Prenatal genetics (2/3): Ultrasound findings (& 2025 ABGC Bootcamp Registration!)
Hello,
This is the 2nd in a series of 3 posts related to prenatal genetics. This month’s post will focus on prenatal ultrasound findings.
We are also excited to announce that registration is open for the 2025 ABGC board review bootcamp, which will take place between June 12th - July 24th, 2025. This bootcamp is for genetic counselors taking the ABGC exam in August 2025. We will cover topics from all 5 domains on the ABGC content outline. An early-bird discount is available through June 1, 2025. For more information and to register, please visit our website.
Please feel free to reach out to me (daniel@studyrare.com) with any questions about the bootcamp or the newsletter. I hope you have a great week!
-Daniel
Questions
Question 94
A woman at 10 weeks gestation presents for an evaluation. This is her first pregnancy, and her blood type is O positive. Ultrasound imaging of her fetus shows a large, multilocular, fluid-filled cavity behind the neck. Which of the following is the most appropriate next step in management?
Question 95
A woman at 20 weeks gestation presents for a second trimester ultrasound. Both she and her partner are known carriers of cystic fibrosis (CF). Which of the following findings on prenatal ultrasound would raise concern that the fetus has CF?
Explanations
Question 94: Offer chorionic villus sampling
Question 95: Echogenic bowel
Ultrasound is an imaging technique used throughout pregnancy to monitor fetal health and to detect fetal anomalies. An ultrasound is like a flashlight 🔦 that uses sound waves (instead of light waves) to illuminate the anatomy of internal structures. Denser structures (like bone) reflect more sound waves and appear brighter (more echogenic), while less dense structures (like fluid) appear darker (less echogenic). The fact that ultrasound is non-invasive, quick to perform, and does not involve radiation exposure makes it ideal for use in the prenatal setting. In addition to looking at the fetus, a prenatal ultrasonographer looks at the placenta, umbilical cord, amniotic fluid volume, uterus, uterine adnexa, and fetal membranes for any abnormalities. Here we will focus on ultrasound anomalies involving the fetus.
Ultrasound imaging of the fetus is divided into fetal biometry and the anatomy survey. Think of these like the vital signs and physical exam, respectively, for the fetus. Fetal biometry measures the length, head size, and estimated fetal weight, while the anatomy survey scans the organ systems of the fetus from head to toe. While major fetal anomalies can be seen in the first trimester, many minor anomalies become visible only as the fetus grows. This is why serial ultrasounds are performed throughout pregnancy.
There are two broad categories of fetal anomalies on prenatal ultrasound: major structural anomalies and “soft markers”. Major structural anomalies, like the large, multilocular, fluid-filled cavity mentioned in Question 94, are clear-cut findings that warrant additional diagnostic testing. This usually involves direct sampling of placental or fetal tissue (discussed further below). In contrast, “soft markers” are more subtle findings that may or may not be connected to an underlying disease process (and that may even self-resolve). In some cases, a “watch and wait” approach can be employed after a soft marker is identified (particularly if there are no other anomalies), though patients may also choose to proceed with diagnostic testing.
Cystic hygroma: An example of a major structural anomaly
The presence of a large, multilocular, fluid-filled cavity near the fetal neck is consistent with a cystic hygroma, which should raise concern for an underlying genetic disorder. Cystic hygromas are lymphatic malformations seen in genetic conditions such as Noonan and Turner syndrome that affect lymphatic development. They can also be seen in trisomies 13, 18, and 21. Given the gestational age of the patient in Question 94, the most appropriate next step is to offer chorionic villus sampling (CVS), a placental biopsy done at 10–13 weeks gestation to test for genetic causes of the cystic hygroma.
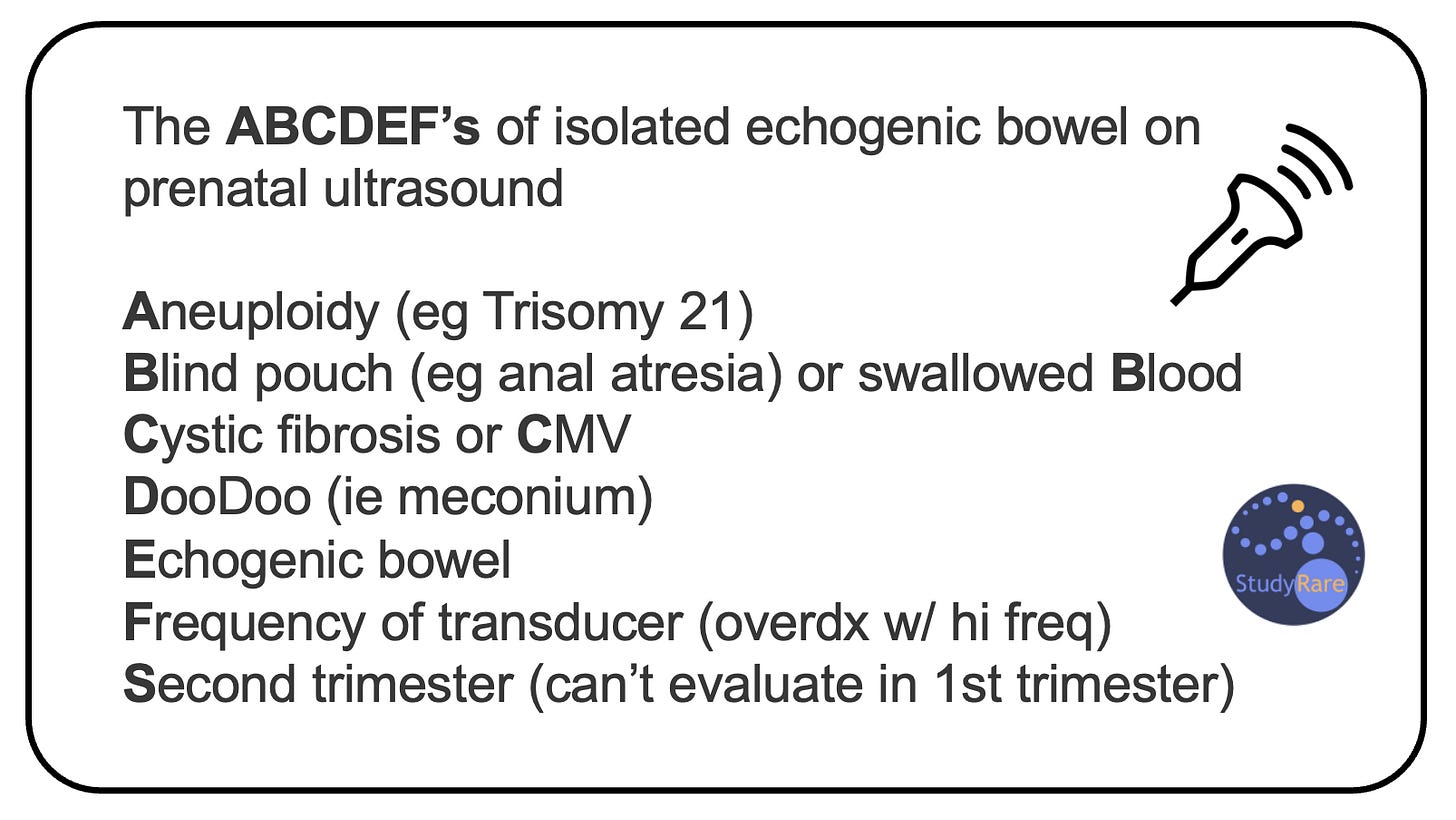
Isolated echogenic bowel: An example of a soft marker
Isolated echogenic bowel (Question 95) is an example of a soft marker seen in the 2nd trimester that is associated with a broad differential diagnosis. Echogenic bowel can be seen in trisomy 21, congenital infections like cytomegalovirus (CMV), and cystic fibrosis. Echogenic bowel may also represent swallowed intra-amniotic blood or dense meconium (fetal stool). In CF, the same chloride channel defect that causes thick, sticky mucus in the lungs also creates viscous intestinal secretions. This results in dense stools that appear bright on the prenatal ultrasound and that obstruct the intestines of newborns with CF (the latter is known as meconium ileus).
Chorionic villus sampling (CVS) versus amniocentesis
CVS and amniocentesis are procedures used to obtain tissue for diagnostic (not screening) purposes. In both cases, a needle is inserted into either the placenta (CVS) or the amniotic sac (amniocentesis) to obtain samples for cell culture and/or genetic testing. CVS can be performed earlier in pregnancy (late 1st trimester) than amniocentesis (early 2nd trimester), which can help if an earlier diagnosis is desired. Because the placenta is mostly derived from the fetus (and not the mother), it is a reliable proxy for genetic testing in the fetus in most cases. However, the placenta can sometimes have a different genetic makeup than the fetus. The term for a genetic abnormality restricted to the placenta is confined placental mosaicism, which can cause genetic test results to differ between the placenta and fetus. Note that NIPT (noninvasive prenatal testing), like CVS, is also a type of genetic testing performed on placental DNA.
💡 Remember that an amniocentesis samples the amniotic fluid (fluid that surrounds the baby), while chorionic villus sampling obtains tissue from the placenta, which contains microscopic projections called chorionic villi.
Incorrect answers (Question 94)
While scheduling a follow-up ultrasound (Choice A) is indicated for monitoring fetal health, the finding of a multilocular cystic hygroma increases the risk of an underlying monogenic disorder and warrants diagnostic testing now. Maternal serum screening for the presence of antibodies against Rh and other blood cell antigens (Choice B) is indicated in cases of suspected immune hydrops fetalis, which can present with increased nuchal translucency and fetal edema (but not a cystic hygroma). The fact that this is the mother’s first pregnancy, along with the mother’s Rh-positive status, also point away from a diagnosis of immune hydrops fetalis. Referral to pediatric surgery (Choice C) is premature without first establishing a diagnosis, as management decisions will depend on the underlying etiology of the findings.
Incorrect answers (Question 95)
The choroid plexus is a structure found within the ventricles of the brain that produces cerebrospinal fluid (CSF). Choroid plexus cysts (CPC, Choice A) form when pockets of CSF become trapped within the choroid plexus. CPC are common and usually benign when present in isolation, though can also be seen in trisomy 18, where they present alongside other findings. CPC are not associated with cystic fibrosis. Single umbilical artery (Choice B) is a soft marker associated with genitourinary defects and may be associated with aneuploidy or fetal growth restriction. A single umbilical artery is not associated with cystic fibrosis. Renal pyelectasis (Choice D), or dilation of the fetal renal pelvis, is often a transient finding and is considered a soft marker for trisomy 21. It is not associated with cystic fibrosis.
Learning objectives
Ultrasound is a technique used throughout pregnancy to monitor fetal well-being and detect fetal anomalies. Fetal anomalies on ultrasound include “soft markers” like echogenic bowel as well as major structural anomalies such as cystic hygromas. Diagnostic testing with chorionic villus sampling (CVS) or amniocentesis should be offered when major structural anomalies are identified on ultrasound in order to look for a genetic basis of the anomalies.
2025 ABMGG General Exam Blueprint | VII. Reproductive Genetics → b) Non-invasive prenatal screening → iii) Ultrasound & c) Invasive prenatal testing
2023 ABGC Exam Content Outline | Domain 3C. Reproductive Risk Management → 3. Prenatal screening & 4. Prenatal diagnostic procedures
Additional resources
A list of fetal anomalies by system (from the fetal medicine foundation)
A table showing examples of major structural anomalies and soft markers by system:






