Hello,
This is the 3rd in a series of 3 posts related to newborn screening. This post will focus on hearing loss. I uploaded a video to YouTube on screening newborns for hearing loss and included an audio voiceover of this newsletter post.
For one more post on newborn screening, have a look at questions 15-16 (December 2022) featuring a newborn screen with an elevated C3.
If you would like to support my work, consider forwarding this newsletter to folks in your network who might be interested in learning more about genetics and rare disease.
Please feel free to email me with any comments or questions about this post (daniel@studyrare.com). If you have suggestions for future posts, please also feel free to reach out!
I hope you are having a great week!
-Daniel
Questions
Question 75
A 2-day-old girl born at term is in the nursery. As part of her routine newborn screen, she undergoes testing for hearing loss, which flags positive. Which of the following techniques was most likely used to screen for hearing loss in the newborn?
Question 76
Follow up testing confirms the presence of hearing loss. Genetic testing is sent, revealing biallelic pathogenic variants in gap junction beta 2 (GJB2), also known as connexin 26. Based on this result, the newborn should be screened with which of the following modalities to look for complications of this condition?
Explanation
Q75: Auditory brainstem response
Q76: No additional screening needed
Approximately 2 in every 1,000 newborns are affected with hearing loss. Screening newborns for hearing loss is important, as the inability to hear can delay the development of language, and treatment strategies such as hearing aids or speech therapy work best when begun early. There are 2 main methods used to screen for hearing loss in newborns: otoacoustic emissions (OAE) and auditory brainstem response (ABR) (Question 75). OAE detects faint sounds given off by the inner ear in response to a sound, while ABR uses electrodes (similar to an EEG) to measure the auditory nerve’s reaction to sounds. Both OAE and ABR are non-invasive and do not require active participation from the newborn, which is essential since they cannot communicate or respond to auditory stimuli as older children or adults can. A table comparing the two screening methods is shown below.
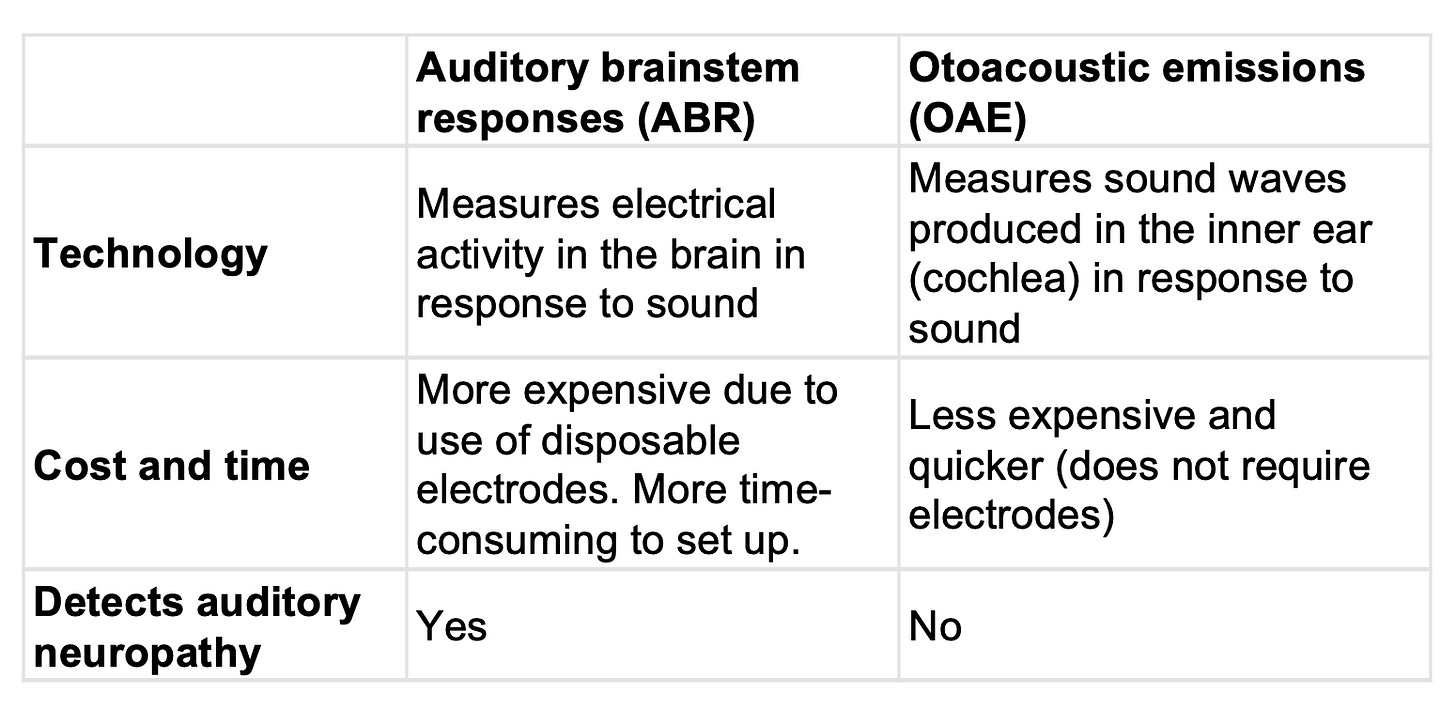
💡 Screening for hearing loss is typically performed in the hospital just prior to discharge. This is because false positives are more likely if the test is performed soon after birth due to the presence of fluid and vernix in the ear canal. In these cases, repeat testing with ABR and/or OAE is recommended (exact protocols vary by hospital and by state) prior to referring to an audiologist or ENT.
Classification of hearing loss
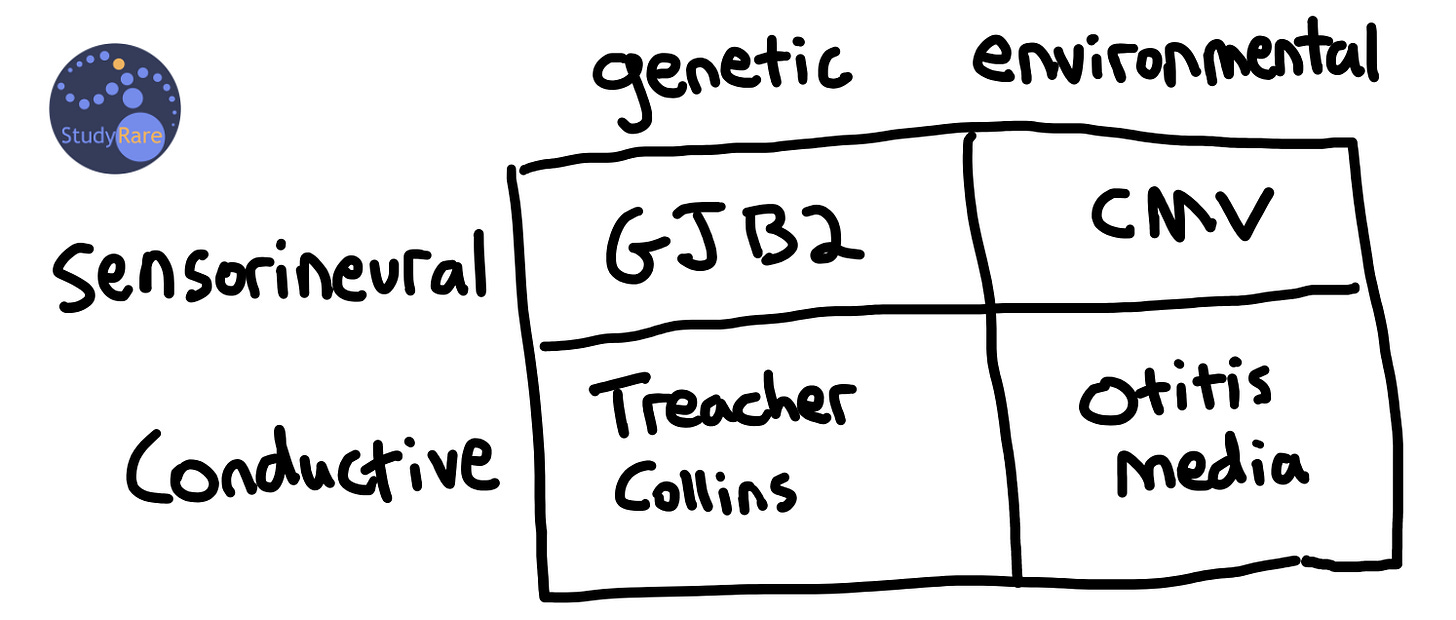
One approach to classifying congenital hearing loss is by genetic versus environmental causes. Genetics accounts for approximately 50% of all cases of hearing loss in newborns and can be further sub-divided into non-syndromic and syndromic causes. The most common non-syndromic cause of congenital hearing loss is GJB2-related hearing loss. Non-syndromic forms of hearing loss are typically autosomal recessive and are not associated with involvement of any other organs outside of the ear, and therefore no additional screening is required in this case (Question 76). In contrast, syndromic forms of hearing loss present with involvement of 1 or more organ systems outside of the ear. Some examples of syndromic hearing loss include Usher syndrome (vision loss), Pendred syndrome (thyroid goiter) and Jervell and Lange-Nielsen syndrome (cardiac arrhythmia). Non-genetic (i.e. “environmental”) factors are also important to consider and include maternal infections during pregnancy (e.g. CMV, Zika), birth trauma, and hyperbilirubinemia.
Hearing loss can also be classified into sensorineural and conductive hearing loss. Sensorineural hearing loss (SNHL) is due to a dysfunction of the cochlea, a sensory organ in the inner ear, or the nerves that transmit hearing signals to the brain (“-neural”). In contrast, conductive hearing loss is due to a physical obstruction or abnormality of the outer or middle ear that prevents sound waves from reaching the inner ear. Patients may also present with mixed forms of both conductive and sensorineural hearing loss.
💡 The cochlea is one of 5 primary sensory organs (along with the retina, tastebuds, skin, and olfactory epithelium) that allows us to navigate our environment. Each of these sensory organs are linked to neurons that fire in response to environmental stimuli and that transmit information about these stimuli to our brain.
Management of hearing loss
Management strategies vary according to both the type of hearing loss the patient presents with and the cultural preferences of the family regarding Deafness. Assistive technologies such as hearing aids, which amplify sound, and cochlear implants, which directly stimulate the auditory nerve, can enhance hearing. If indicated, surgery can be performed to repair the ossicles, the bones of the middle ear, or a ruptured eardrum. In addition, various types of sign language exist throughout the world that enable people to communicate without spoken words. It is important to recognize that perspectives on hearing loss management vary widely. Some individuals within the Deaf community do not perceive hearing loss as a condition requiring "treatment" but rather as an integral aspect of their identity.
Incorrect answers (Question 75)
Hearing loss can present at any age and is most likely to impact development when present at an early age. Thus, screening for hearing loss in childhood is often performed through the child’s school or as part of a well-child visit and typically consists of pure tone audiometry (PTA) (Choice A). PTA involves the child listening for beeps at various pitches and volumes through headphones and indicating when they hear them. Newborns are too young to have reliable responses to traditional PTA, which makes it difficult to use this method in this population. Electronystagmography (Choice B) is a diagnostic test used to evaluate the vestibular system, the part of the inner ear that helps control balance. This test measures involuntary eye movements (nystagmus) that can occur as a result of a balance disorder and does not directly measure hearing loss. Pneumatic otoscopy (Choice C) is used to assess the eardrum's mobility, which can be affected by conditions that result in fluid accumulation in the middle ear (e.g. infections). While pneumatic otoscopy can provide valuable information about the presence of middle ear pathologies that may impact hearing, it does not directly measure hearing sensitivity.
Incorrect answers (Question 76)
Patients with CHARGE syndrome, which is due to pathogenic variants or deletion of CHD7, can have congenital hearing loss along with congenital heart defects that may warrant a screening echocardiogram (Choice A). Pendred syndrome is due to variants in SLC26A4 and can cause congenital hearing loss and an enlarged goiter that typically presents in teenagers. A thyroid ultrasound (Choice B) may be warranted in these cases. In a patient with GJB2-related hearing loss, an MRI of the brain with views of the internal auditory canal (Choice C) would be expected to be normal in most cases. Inner ear abnormalities on brain MRI may be seen if performed on a patient with CHARGE syndrome (dysplasia of the semicircular canals) or Pendred syndrome (enlarged vestibular aqueducts).
Learning objectives
Identifying hearing loss in newborns is important, as the inability to hear can delay the development of language.
The two main screening methods for hearing loss in newborns include OAE and ABR.
Hearing loss can be classified as sensorineural or conductive, syndromic or non-syndromic, and may be due to genetic and/or environmental factors.
Management of deafness may include hearing aids, surgery for cochlear implants or ossicle repair, and speech therapy that includes teaching sign language. Interventions for hearing loss work best when begun early.
2023 ABMGG General Exam Blueprint | IX. Population screening → a. Newborn screening → ii) Other screening | V. Single gene inheritance → d. Single gene disorders → viii) Deafness
2023 ABGC Exam Content Outline | Domain 1C. Genetic Conditions → 3. Screening, surveillance, and risk reduction | Domain 3A. Testing and Interpretation → 1. Test methodologies/technologies and applicable limitations
References
Hearing Loss Screening: Recommendations and Guidelines (CDC)
Hearing Assessment in Infants, Children, and Adolescents: Recommendations Beyond Neonatal Screening



